Oxford R21/Matrix-M™ malaria vaccine receives WHO recommendation for use paving the way for global roll-out
The highly effective vaccine developed by the University of Oxford and the Serum Institute of India, leveraging Novavax’s adjuvant is critical to reducing over half a million malaria-related deaths annually.

R21 Vaccinations at Tanzania clinical site - Photo Credit Tom Wilkinson, University of Oxford.
- R21/Matrix-M™ malaria vaccine has been recommended for use by the World Health Organization’s Strategic Advisory Group of Experts (SAGE) and the Malaria Policy Advisory Group (MPAG)
- Developed by The University of Oxford and the Serum Institute of India, leveraging Novavax’s adjuvant technology, R21/Matrix-M™ malaria vaccine demonstrates high efficacy with a reassuring safety profile
- The R21/Matrix-M™ malaria vaccine is an easily deployable vaccine that can be manufactured at mass scale and modest cost, enabling as many as hundreds of millions of doses to be supplied to countries which are suffering a significant malaria burden
- The Serum Institute of India has already established production capacity for 100 million doses per annum, which will be doubled over the next two years
- The World Health Organization's recommendation today is required for UNICEF to procure and GAVI to purchase the vaccine, paving the way for vaccination of children in populations most at risk
- R21/Matrix-M™ malaria vaccine marks the culmination of 30 years of malaria vaccine research at the University of Oxford's Jenner Institute
Recommendations from WHO
The R21/Matrix-M™ malaria vaccine developed by the University of Oxford and the Serum Institute of India, leveraging Novavax’s adjuvant technology, has been recommended for use by the World Health Organization (WHO) after meeting required safety, quality and effectiveness standards.
Following a rigorous, detailed scientific review by the WHO’s independent advisory body, the Strategic Advisory Group of Experts (SAGE) and the Malaria Policy Advisory Group (MPAG), the R21/Matrix-M™ malaria vaccine has been recommended for use. The recommendation was based on pre-clinical and clinical trial data which showed good safety and high efficacy in four countries, at sites with both seasonal and perennial malaria transmission, making it the world’s second-ever WHO recommended vaccine for preventing malaria in children.
The vaccine was developed by the Jenner Institute at Oxford University and Serum Institute of India with support from the European and Developing Countries Clinical Trials Partnership (‘EDCTP’), the Wellcome Trust, and the European Investment Bank (‘EIB’). To date the R21/Matrix-M™ malaria vaccine has been licensed for use in Ghana, Nigeria and Burkina Faso. In combination with public health measures such as the use of insecticide-treated bed nets, this vaccine can help save and improve the lives of millions of children and their families.
The vaccine has recently reached the primary one-year endpoint in a pivotal large-scale Phase III clinical trial – funded mainly by the Serum Institute of India, with Oxford University as the regulatory sponsor – including 4,800 children across Burkina Faso, Kenya, Mali and Tanzania. The Phase III trial results are under peer review before publication.
The vaccine was well tolerated with a good safety profile. The efficacy of the vaccine over 12 months was 75% (95% CI 71-79; p<0.001) at sites with high seasonal malaria transmission and 68% (61-74; p<0.001) at the sites with more perennial transmission using standard age-based administration.
There was some waning of efficacy over the first year of follow-up at both seasonal and perennial transmission sites, but a booster dose restored efficacy at the seasonal sites with a vaccine efficacy over 18 months of 74% (70-77; p<0.001).
Significantly higher vaccine-induced antibody titres were observed in the 5–17-month age group compared with 18–36-month-olds (p<0.0001). The younger age group, in whom this vaccine is most likely to be widely deployed, showed the highest 12-month vaccine efficacy at both seasonal, 79% (73-84, p<0.001), and standard sites, 75% (65-83, p<0.001).
In a previous Phase IIb clinical trial conducted in Burkina Faso, Oxford researchers and their partners reported 2 year efficacy and showed that that a booster dose of R21/Matrix-M™ maintained high efficacy against malaria and continued to meet the World Health Organization’s Malaria Vaccine Technology Roadmap goal of a vaccine with at least 75% efficacy. This followed earlier results from the same trial reporting 1 year efficacy of 77%.
The Phase III results improve understanding of how vaccine efficacy varies with age and across regions in relation to transmission intensity and seasonality. Further studies are also exploring optimal dosing schedules and tracking long-term immune response.
Prof. Adrian Hill, Director of The Jenner Institute, & Lakshmi Mittal and family Professor of Vaccinology, University of Oxford said: 'The R21/Matrix-M™ malaria vaccine has been shown to be safe and highly effective across multiple clinical studies and is now approved as WHO policy for widespread use. The vaccine is easily deployable, cost effective and affordable, ready for distribution in areas where it is needed most, with the potential to save hundreds of thousands of lives a year.’
Dr Mehreen Datoo, Academic Clinical Fellow in Infectious Diseases & Microbiology at The Jenner Institute, University of Oxford said: 'The University of Oxford has one of the most active malaria vaccine programmes in the world, with thanks to a network of global collaborators. Today’s achievement would not be possible without the efforts of our international partners, their incredible field teams, and of course, the participants and their caregivers. This is a significant milestone in the fight against malaria but there is still more to do – we are already working on new vaccine candidates to target other malaria parasites and clinical trials focussed on eradication of malaria.’
Dr Lisa Stockdale, Senior Immunologist, The Jenner Institute, University of Oxford said: 'Today’s news is testament to the work of our small but dedicated team and means we have another tool with which to fight this disease that kills over half a million people every year. However, further work is critical to establish not just that the vaccine works, but to understand more about how it works, and apply that knowledge to future vaccines.’
Adar Poonawalla, CEO of the Serum Institute of India, said: 'For far too long, malaria has threatened the lives of billions of people across the globe, disproportionately affecting the most vulnerable amongst us. This is why the WHO recommendation and approval of the R21/Matrix-M™ vaccine marks a huge milestone on our journey to combat this life-threatening disease, showing what exactly can be achieved when the public and private sector, scientists and researchers, all work together towards a shared goal.’
'As we continue to work together to create a healthier, more equitable world for everyone, I am incredibly proud of the part that the Serum Institute of India has played in developing the R21 malaria vaccine. We look forward to scaling up the vaccine production to ensure that it is accessible to those who need it the most.'
John C. Jacobs, President and Chief Executive Officer, Novavax said: 'This WHO designation highlights the meaningful contribution that R21/Matrix-M™ is likely to have in accelerating and expanding access to a safe, efficacious and potentially life-saving vaccine to control malaria – a disease that disproportionately impacts children. Novavax celebrates the importance of this milestone and is proud of the role of our saponin-based Matrix-M™ adjuvant plays in the R21/Matrix-M™ malaria vaccine, which has now met the rigorous standards required for WHO recommendation.'
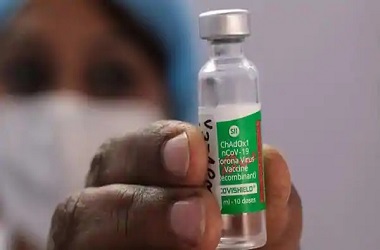
Cost and Manufacturing Capacity
The R21/Matrix-M™ vaccine is licensed to the Serum Institute of India, the world’s largest vaccine manufacturer as well as a long-term partner of Oxford University. Notably, the Serum Institute has already established production capacity for 100 million doses per annum, which will be doubled over the next two years. This scale of production is critical because vaccinating those at high risk of malaria will be important in stemming the spread of disease, as well as protecting the vaccinated.
The Matrix-M component is a proprietary saponin-based adjuvant from Novavax, which is licensed to the Serum Institute for use in endemic countries, while Novavax retains commercial rights in non-endemic countries.
Vaccine Roll-Out
With the approval and recommendations by the WHO, additional regulatory approvals are expected to follow shortly and R21/Matrix-M vaccine doses could be ready to begin wider roll-out as early as next year.
Notes to editors:
For further information or to arrange an interview, please contact the University of Oxford press office at news.office@admin.ox.ac.uk or on +44 (0)1865 280528 OR Dr. Adriaan Louis Taljaard, Manager Strategic Communications (Vaccines) on Adriaan.taljaard@admin.ox.ac.uk.
Video footage and b-roll is available here: https://vimeo.com/showcase/10684363
(Password: “R21”)
Please credit: University of Oxford
Images are available here: https://www.dropbox.com/sh/q9mzu3lnn14t2lo/AAAca_qLkwkzlL9TQaJe0fq4a?dl=0
Please credit: University of Oxford
Video for embed is available here: WHO approves Oxford vaccine against malaria
Supplementary information:
1) Link to R21/Matrix-M™ malaria vaccine phase III trial results pre-print paper
2) Links to other related R21 vaccine publications
3) Link to Five things you need to know about the new R21 malaria vaccine
About the University of Oxford
Oxford University has been placed number 1 in the Times Higher Education World University Rankings for the eighth year running, and number 3 in the QS World Rankings 2024. At the heart of this success are the twin-pillars of our ground-breaking research and innovation and our distinctive educational offer.
Oxford is world-famous for research and teaching excellence and home to some of the most talented people from across the globe. Our work helps the lives of millions, solving real-world problems through a huge network of partnerships and collaborations. The breadth and interdisciplinary nature of our research alongside our personalised approach to teaching sparks imaginative and inventive insights and solutions.
Through its research commercialisation arm, Oxford University Innovation, Oxford is the highest university patent filer in the UK and is ranked first in the UK for university spinouts, having created more than 300 new companies since 1988. Over a third of these companies have been created in the last five years. The university is a catalyst for prosperity in Oxfordshire and the United Kingdom, contributing £15.7 billion to the UK economy in 2018/19, and supports more than 28,000 full time jobs.
About The Jenner Institute
The Jenner Institute, which is where the Oxford-AstraZeneca-Serum Institute Covid-19 vaccine was designed and first made, is based within the Nuffield Department of Medicine, University of Oxford, and operates out of the Old Road Campus Research Building, in Headington, Oxford. The Jenner Institute also supports senior vaccine scientists, known as Jenner Investigators, within many other departments across the University of Oxford, as well as externally with The Pirbright Institute in Surrey, UK. The Jenner Institute brings together investigators who are designing and developing numerous vaccines to generate an exceptional breadth of scientific know-how and critical mass, whilst still allowing the individual investigators to remain independent and accountable to their funders and stakeholders.
The Jenner Institute is supported by the Jenner Vaccine Foundation, a UK registered charity and is advised by the Jenner Institute Scientific Advisory Board.
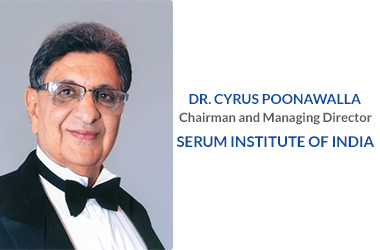
About the Serum Institute of India Pvt Ltd (SIIPL)
Serum Institute of India Pvt. Ltd, is a global leader in vaccine manufacturing, dedicated to providing affordable vaccines worldwide. Present across 170+ countries, including the US, UK, and Europe, SII holds the distinction of being the world's largest vaccine manufacturer. SII's multifunctional production and one-of-the-largest facility in Manjri, Pune, with an annual capacity of 4 billion doses, has saved over 30 million lives over the years.
Founded in 1966, SII's primary mission is to produce life-saving immunobiological drugs, with a particular emphasis on affordability and accessibility. Guided by a strong commitment to improving global health, the company has played a pivotal role in reducing the prices of essential vaccines, such as Diphtheria, Tetanus, Pertussis, HIB, BCG, r-Hepatitis B, Measles, Mumps, and Rubella. Notably, they are the manufacturers of 'Pneumosil,' the world's most affordable PCV, and the first indigenous qHPV vaccine in India. Moreover, SII has been at the forefront of the global fight against COVID-19, delivering over 2 billion doses of the COVID-19 vaccine worldwide.
To further expand its global presence and ensure widespread vaccine availability, SII has established Serum Life Sciences Ltd, a subsidiary in the UK. Through relentless pursuit of innovation, SII continues to champion the cause of affordable vaccines, making a positive impact on the lives of millions worldwide. www.seruminstitute.com
About Novavax
Novavax, Inc. (Nasdaq: NVAX) promotes improved health by discovering, developing and commercializing innovative vaccines to protect against serious infectious diseases. Novavax, a global company based in Gaithersburg, Md., U.S., offers a differentiated vaccine platform that combines a recombinant protein approach, innovative nanoparticle technology and Novavax's patented Matrix-M adjuvant to enhance the immune response. Focused on the world's most urgent health challenges, Novavax is currently evaluating vaccines for COVID, influenza, and COVID and influenza combined. Please visit novavax.com and LinkedIn for more information.
About the WHO
The World Health Organization (WHO) plays a singular role in leading the global health ecosystem, producing technical guidelines and tools to prevent and treat disease, and acting as a country-level convener with an unparalleled level of trust. The crises of the 21st century, including COVID-19, have made clear both the inequity of access to effective and affordable healthcare and the indispensable role of WHO. Yet WHO lacks sufficient resources to fulfill its mandate. And, beyond funding, its vision cannot be achieved by the public sector alone. The WHO Foundation was created as an independent Swiss foundation affiliated with but independent of WHO to marshal new resources from philanthropists, foundations, businesses, and individuals to support its mission: promote health, keep the world safe, and serve the vulnerable.